High pressure ventilator alarm causes are a common challenge in critical care settings, prompting healthcare professionals to navigate complex troubleshooting and management strategies. This comprehensive guide delves into the underlying mechanisms, potential causes, and effective management techniques for high pressure ventilator alarms, providing a valuable resource for optimizing patient care and ensuring respiratory support.
High-Pressure Ventilator Alarm Causes
High-pressure ventilator alarms are triggered when the pressure within the ventilator circuit exceeds a predetermined threshold. These alarms are crucial for patient safety, as excessively high pressures can cause barotrauma, volutrauma, and other complications.
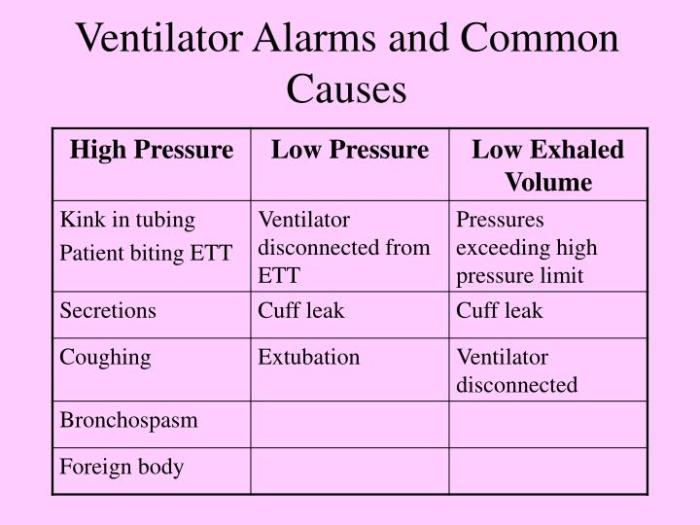
The most common causes of high-pressure ventilator alarms include:
- Excessive airway resistance:This can be caused by bronchospasm, mucus plugging, or a kinked endotracheal tube.
- Inadequate lung compliance:This can be caused by pulmonary edema, fibrosis, or atelectasis.
- Increased airway secretions:This can occur in patients with excessive secretions or those who are not receiving adequate suctioning.
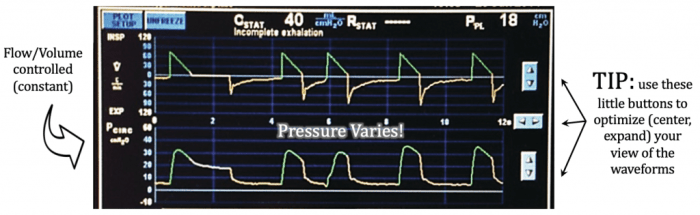
- Incorrect ventilator settings:This can include settings such as a high peak inspiratory pressure (PIP), a low positive end-expiratory pressure (PEEP), or a short inspiratory time.
It is important to note that high-pressure ventilator alarms can also be caused by equipment malfunctions, such as a faulty pressure transducer or a leak in the ventilator circuit.
Alarm Management Strategies
Effective management of high-pressure ventilator alarms is crucial to ensure patient safety and adequate ventilation. This involves differentiating between true and false alarms and adjusting ventilator settings appropriately.
Differentiating True and False Alarms
Differentiating between true and false alarms is essential. True alarms indicate an actual problem with the ventilator or patient’s condition, while false alarms occur due to transient events or inappropriate settings.
- True alarms may be caused by:
- Airway obstruction
- Bronchospasm
- Pneumothorax
- False alarms may be caused by:
- Inadequate patient-ventilator synchrony
- Improper airway humidification
- Ventilator malfunction
Adjusting Ventilator Settings
Once the type of alarm is determined, appropriate adjustments to ventilator settings can be made to resolve high-pressure alarms while maintaining adequate ventilation.
- For true alarms, the underlying cause should be addressed first.
- For false alarms, adjusting settings such as:
- Increasing the inspiratory flow rate
- Reducing the inspiratory time
- Using a higher PEEP
may help resolve the alarm.
Troubleshooting High-Pressure Alarms
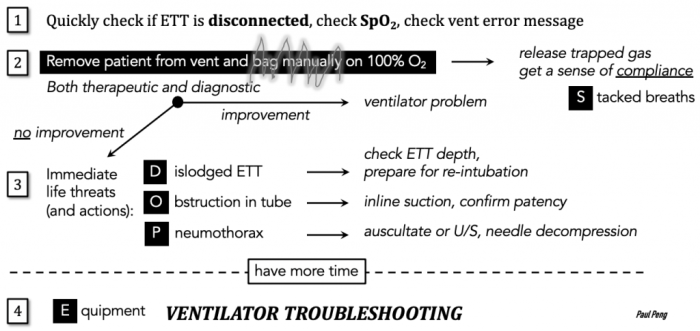
High-pressure alarms on ventilators are crucial safety mechanisms that indicate excessive pressure within the patient’s respiratory system. To effectively manage these alarms, it is essential to implement a systematic troubleshooting approach.
Step-by-Step Troubleshooting Guide
- Assess the Patient’s Condition:Verify the patient’s respiratory status, airway patency, and chest expansion.
- Check Ventilator Settings:Ensure that the ventilator settings, including pressure limits, tidal volume, and respiratory rate, are appropriate for the patient’s condition.
- Inspect the Circuitry:Examine the ventilator circuit for any leaks, obstructions, or kinks that could cause pressure buildup.
- Check the Pressure Sensor:Verify the calibration and functionality of the pressure sensor to ensure accurate pressure readings.
- Inspect the Expiratory Valve:Examine the expiratory valve for proper function and ensure it is not obstructed or leaking.
- Evaluate the Patient’s Secretions:Assess the patient’s secretions and consider suctioning if excessive secretions are present.
- Check for Pneumothorax:Auscultate the patient’s lungs and check for any signs of pneumothorax, which can cause increased intrathoracic pressure.
Common Error Codes and Troubleshooting Actions
| Error Code | Troubleshooting Actions |
|---|---|
| E01 | Pressure sensor malfunction. Check sensor calibration and connections. |
| E02 | Circuit leak. Inspect the circuit for leaks, kinks, or obstructions. |
| E03 | Expiratory valve malfunction. Check the valve for proper function and ensure it is not obstructed. |
| E04 | Pneumothorax. Auscultate the patient’s lungs and assess for signs of pneumothorax. |
Patient Factors Contributing to High-Pressure Alarms
Patient-related factors can significantly contribute to the occurrence of high-pressure ventilator alarms. Understanding these factors is crucial for effective alarm management and ensuring optimal patient care.
Increased airway resistance is a common patient factor that can lead to high-pressure alarms. Conditions such as bronchospasm, secretions, or airway narrowing can obstruct airflow, resulting in increased resistance and pressure buildup within the ventilator circuit. Similarly, decreased lung compliance, often seen in conditions like pulmonary edema or fibrosis, reduces the lungs’ ability to expand and recoil, leading to higher airway pressures.
Patient Positioning and Interventions, High pressure ventilator alarm causes
Proper patient positioning can play a role in mitigating high-pressure alarms. Elevating the head of the bed, for example, can promote lung expansion and reduce airway resistance. In addition, interventions like suctioning to remove secretions or administering bronchodilators to relax airway muscles can help improve airflow and reduce pressure.
Prevention of High-Pressure Ventilator Alarms
High-pressure ventilator alarms are a common occurrence in the intensive care unit, and they can be a source of significant stress for clinicians. By implementing a comprehensive prevention plan, clinicians can minimize the risk of these alarms and improve patient outcomes.
Key measures to prevent high-pressure ventilator alarms include optimizing ventilator settings, ensuring proper patient positioning, and managing the airway effectively. Clinicians should also be aware of the patient factors that can contribute to high-pressure alarms, such as increased airway resistance or decreased lung compliance.
Ventilator Settings
- Set the tidal volume to the lowest possible level that provides adequate ventilation.
- Set the respiratory rate to the lowest possible level that maintains adequate oxygenation and carbon dioxide removal.
- Use a pressure-limited ventilation mode to prevent excessive airway pressures.
- Use a positive end-expiratory pressure (PEEP) to keep the airways open and reduce the risk of atelectasis.
Patient Positioning
- Position the patient in a semi-recumbent position to promote lung expansion.
- Avoid positioning the patient in a prone position, as this can increase airway resistance.
- Use pillows or other supports to keep the patient’s head and neck in a neutral position.
Airway Management
- Use an endotracheal tube or tracheostomy tube that is the appropriate size for the patient.
- Suction the airway regularly to remove secretions.
- Humidify the airway to prevent drying and irritation.
Patient Factors
- Be aware of patient factors that can contribute to high-pressure alarms, such as increased airway resistance or decreased lung compliance.
- Monitor the patient’s respiratory status closely and make adjustments to the ventilator settings as needed.
- Consider using bronchodilators or other medications to improve airway function.
Questions Often Asked: High Pressure Ventilator Alarm Causes
What are the most common causes of high pressure ventilator alarms?
High pressure ventilator alarms can be caused by various factors, including increased airway resistance due to bronchospasm, mucus plugging, or endotracheal tube kinking; decreased lung compliance due to pulmonary edema, fibrosis, or atelectasis; and excessive tidal volumes or positive end-expiratory pressure (PEEP).
How can I differentiate between true and false high pressure ventilator alarms?
True high pressure alarms indicate a genuine increase in airway pressure, while false alarms occur when the ventilator senses a pressure spike that is not reflective of actual airway pressure. False alarms can be caused by leaks in the ventilator circuit, faulty sensors, or improper calibration.
What are some effective strategies for managing high pressure ventilator alarms?
Managing high pressure ventilator alarms involves identifying and addressing the underlying cause. This may include adjusting ventilator settings, such as reducing tidal volume or PEEP, optimizing patient positioning to improve lung expansion, and administering bronchodilators or mucolytics to reduce airway resistance.